Introduction
Multiple sclerosis (MS) is an inflammatory neurodegenerative disorder of the human central nervous system. Patients with MS typically present between the ages of 20-40 years, with affected women outnumbering men (2:1), and the progressive phase of disease manifests anytime between 5–35 years after the onset [1]. Neurologists suggest that MS patients may be grouped into four classes including relapsing-remitting MS (RRMS) as the most common class comprising about 85% of MS patients, secondary progressive MS (SPMS), primary progressive MS (PPMS) about 10% of MS patients and progressive-relapsing MS (PRMS) as an uncommon form [2]. MS usually begins as a relapsing, episodic disorder (relapsing-remitting multiple sclerosis), evolving into a chronic neurodegenerative condition characterized by progressive neurologic disability [3]. It has been suggested that Iran has a moderate to high MS outbreak rate [4]. Various studies have shown that genetics and heredity play a role in response to the treatment of MS and almost 10–15% of cases occur in first-degree relatives of patients with MS [1, 5]. The risk of occurrence of this complex illness is related to exposure to environmental factors in genetically susceptible individuals [6]. Development in statistical methods of analysis and a growing consensus that individual genetic variation likely influences therapeutic responses has made the search for biomarkers in MS as a very active field of investigation [7]. MicroRNAs (miRNAs) have recently transpired as potential biomarkers of disease in various autoimmune disorders including rheumatoid arthritis and systemic lupus erythematosus. Moreover, data demonstrate that miRNA dysregulation may contribute to the pathogenesis of MS [8]. miRNAs are short non-coding RNA molecules almost with 19-25 nucleotides which help to the control of various biological processes [9]. miRNAs control the gene expression at the post-transcriptional level by binding to the 3′-untranslated region (UTR) or 5´UTR of their mRNA targets, leading to blockage or degradation of target messenger RNAs (mRNA) [10-11]. In MS disease, miRNAs dysregulation is mostly presented in various immune cells, but less knowledge is accessible on circulating miRNAs that apply strong biomarker potential because of their exceptional stability in body fluids [12]. miRNAs exist in a constant form in human blood and plasma, and their expression profiles can be easily examined, making them ideal MS biomarker candidates [13]. Using the miRWalk 2.0 database, miR-377 and miR-98 were selected as an appropriate and involved miRNAs in MS disease [14]. Therefore, we focused on miR-377 and miR-98 as two miRNAs involved in MS. The expression of miR-377 and miR-98 was evaluated by quantitative real-time polymerase chain reaction (RT-PCR) in peripheral blood mononuclear cells of RRMS patients (recurring patients and two months after relapse patients) and controls. Our purpose was to investigate the expression of circulating miR-377 and miR-98 as biomarkers in RRMS to gain a deeper understanding of the role of these miRNAs in RRMS for future investigations.
Materials and Methods
Participants
In this case-control investigation, blood samples were collected from 60 RRMS patients, of which 30 were recurrent and 30 patients had recurrences for at least two months, and had referred to MS Clinic of Kashani Hospital, Isfahan Province, as well as 30 random samples from healthy subjects (both male and female). The latter had no history of autoimmune disease based on the physician examination. Recurring patients and two months after relapse patients were diagnosed by an expert a neurologist based on the recommended McDonald diagnostic criteria [15]. Thirty-two patients had only received interferon (IFN)-β treatment, whilst all the other patients had received no treatment in two months prior to sampling. Four ml blood was collected in ethylenediamine tetraacetic acid-containing tubes and immediately transported on ice to the laboratory. Written informed consent was obtained from all the participants prior to sample collection. The study was approved by the Ethics Committee of the Medical Genetics Research Center of Genome, Isfahan, Iran.
Peripheral blood mononuclear cell isolation
Isolation of mononuclear cells was used based on density gradient lymphoprep (Bio Sera, USA) according to the brochure. Generally, 4 ml of blood was diluted by physiological saline with equal ratio and added slowly to the 4 ml lymphoprep solution. Mononuclear cells, monocytes, and lymphocytes were separated in a middle phase. These falcons were centrifuged at 800 g, 30 min at 25oC, and then from the middle phase, peripheral blood mononuclear cells were transferred into a 2 ml RNAase-free microtube and frozen at -70oC until the next step.
miRNA extraction and complementary DNA preparation
RNA Hybrid-R kit (Geneall, Korea) was used for miRNA extraction and tested by a NanoDrop spectrometer (Thermo Scientific, USA) for the value of RNA quality with the absorbance of 260/280 nm. Complementary DNA (cDNA) was synthesized by poly-A tailing with the standard kit (Pars Genome, Iran) according to the brochure applied.
Real-time polymerase chain reaction (RT-PCR)
The real-time quantitative PCR reactions were performed with a final volume of 10 μl by a Rotor-Gene 6000 system (Corbett Life Science, Mortlake, Australia). Generally, 20 ng μL−1 of the product of cDNA was added to 10 pmol μL−1 of primers of miR-377 and miR-98 in master mix (Pars Genome, Iran) and 5 m of SYBR premix ExTaq II (TaKaRa, Kusatsu, Shiga Prefecture, Japan) and U6 as a housekeeping gene (Pars Genome, Iran) was selected for normalization of the data. Thermal steps PCR were in the form 95˚C for 15 min, 40 cycles of 95˚C for 15 s, 60˚C for 30 s, and 72˚C for 30 s. Real-time PCR data analysis was performed using the 2-ΔΔCT method [16]. Triplicate experiments were applied and negative controls lacking template were run with all reactions.
Statistical analysis
Graph Pad Prism statistical software version 8.2.0 (Graph Pad, San Diego, CA, USA) and measurement of normalization by the Kolmogorov-Smirnov test and one-way ANOVA were applied for the statistical analysis. Statistical significance was set at the p<0.05.
Results
Biological features of participants
In this study, 90 samples including 60 patients with RRMS, 30 of whom were recurring patients (mean age: 39.20±2.154 years, range: 18-60, 7 males and 23 females), 30 were two months after relapse patients (mean age: 33.7±1.522; range: 21-45; 9 males and 21 females), and 30 healthy subjects (mean age: 38.60±1.843; range: 21-58; 10 males and 20 females) were investigated. RRMS patients and healthy individuals were matched in terms of age and sex. There was no significant difference in the type of drug treatment (interferon and non-interferon) (p=0.388). Biological and clinical features of participants can be observed in table 1.
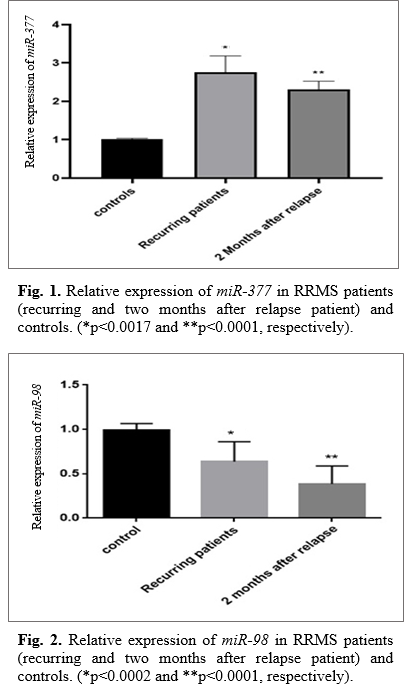
Up-regulation of miR-377
In order to analyze of relative miRNA expression, data were analyzed using 2−ΔΔCt method. We observed a statistically significant increase in the level of miR-377 between the RRMS patients (recurrent and two months after relapse) and healthy subjects. The data has indicated the relative quantification (RQ) being different in studied groups (p=0.0017 and p=0.0001, respectively). As seen in Figure 1, the expression level of miR-377 in recurrent patients was higher than the two months after relapse patients.
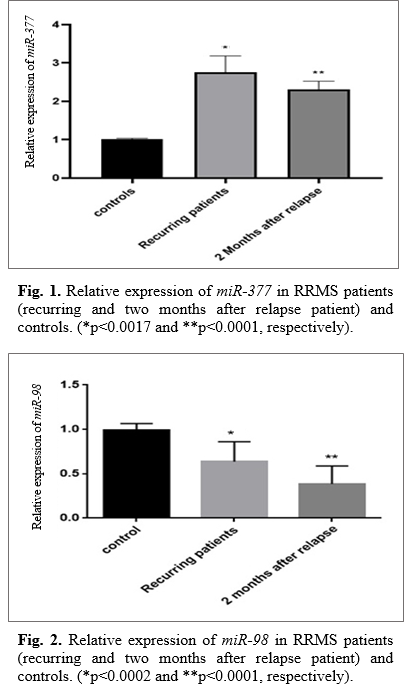
Down-regulation of miR-98
To display the vital role of miR-98 in RRMS patients, qRT-PCR was used in the level of expression of miR-98 in studied groups. Even though our results demonstrated down-regulation in the expression of miR-98 in patients compared to healthy subjects (p=0.0002 and p=0.0001, respectively), however, there was a higher decrease in miR-98 expression in two months after relapse patients compared with the recurrent patients (Fig. 2).
Table 1. Biological and clinical features of the participants
| Characteristics |
Controls |
Recurring patients |
Two months after relapse patients |
| Number of subjects |
30 |
30 |
30 |
| Mean age (years) |
38.60±1.843 |
39.20±2.154 |
33.7±1.522 |
| Range |
21-58 |
18-60 |
21-45 |
| Drug: |
|
|
|
| Interferon |
- |
21 |
11 |
| Non-interferon |
- |
9 |
19 |
| Family history |
- |
12 |
8 |
Discussion
MS, a repeated cause of neurological disease arising in the early to middle adulthood, has a complex etiology involving both genetic and environmental factors. Recent years have shown major progress in the dissection of the fundamental genetic etiology underlying MS risk [17]. Recognition of reliable biomarkers for MS bears the potential for better diagnosis of MS, progression, and evaluation of treatment responses. However, identification of appropriate biomarker sets for MS based on parameters in peripheral blood is only in its infancy [18]. Several investigations have recently explored the involvement of miRNAs in MS using a diversity of miRNA profiling techniques and they have proposed miRNAs as potential biomarkers in MS [19]. Therefore, miR-377 and miR-98 were selected from the miRWalk 2.0 database as two miRNAs involved in MS disease. We assessed whether the expression of miR-377 and miR-98 associates with RRMS and also the possible use of these miRNAs as diagnostic biomarkers for the disease. We detected the miR-377 and miR-98 expression by real-time qPCR in RRMS patients (recurrent and two months after relapse) compared to the controls. Selected miRNAs were analyzed in peripheral blood mononuclear cells after isolating them. Our findings showed increased expression of miR-377 in both recurring patients and two months after relapse patients. Therefore, up-regulation of miR-377 can be a potential therapeutic target to inhibit RRMS progression in future investigations. On the other hand, data indicated that the expression of miR-98 decreased significantly in recurring patients and two months after relapse patients in comparison with controls. Perhaps, down-regulation of miR-98 in the RRMS groups in comparison with the control has a tumor-suppressing role in RRMS. It was shown miR-377-5p levels being positively correlated with serum amyloid A circulating levels. The levels of miR-377-5p increased in patients presenting increased serum amyloid A levels [20]. Recently, many studies have shown that transforming growth factor-β (TGF-β) regulates specific miRNAs to regulate fibrosis in various diseases. Recent reports demonstrate that TGF-β1 is capable of inducing miR-377 becoming consistently up regulated [21]. Up-regulation of miR-377 has been observed in animal models of diabetic nephropathy and may be induced under the condition of high glucose and by TGF-β1 [22]. We also observed up-regulation of miR-377 in both groups studied. An earlier study using miRNA microarray analysis showed that 26 miRNAs such as miR-98 are significantly down-regulated in peripheral blood of patients with all MS subtypes including primary progressive, secondary progressive and relapsing-remitting disease [23]. It has been proposed that miR-98 as a miRNA biomarkers involved in the therapeutic response in MS has been reduced affected by the GSK3𝛽 drug [24]. It has also been indicated that miR-98 expression profile decreases in peripheral blood mononuclear cells of human systemic lupus erythematosus [25]. Additionally, our data revealed down-regulation of miR-98, in RRMA patients. The use of miR-377 and miR-98 as therapeutic factors, is a new strategy for restoring and maintaining neuronal function during neuro-degenerative disorders such as MS. We studied the correlation of the expression of two miRNAs (miR-377 and miR-98) in RRMS. It can be assumed that these miRNAs may have an important role in RRMS. This means that in the future, miR-377 and miR-98 can be considered as potential biomarkers for the early diagnosis of RRMS patients. Understanding the complexity of miRNAs may open up a new way to find biomarkers for clinical diagnosis of some serious diseases and to monitor the efficacy of various therapies.
Conclusion
In conclusion, the expression of miR-377 and miR-98 were significantly different in RRMS patients compared with controls. The results suggest that these miRNAs may be of relevance with a human autoimmune disease like MS. Further studies on the effects of miRNAs can lead to new treatment strategies concerning neuroinflammatory diseases.
Conflict of Interest
The authors declared that they have no conflict of interest.
Acknowledgement
This study was supported by Medical Genetics Research Center of Genome, Isfahan, Iran.
References
- Ransohoff RM, Hafler DA, Lucchinetti CF. Multiple sclerosis-a quiet revolution. Nat Rev Neurol. 2015; 11(3): 134-42.
- Goldenberg MM. Multiple sclerosis review. Pharmacy and Therapeutics. 2012; 37(3): 175-79.
- Hauser SL, Waubant E, Arnold DL, Vollmer T, Antel J, Fox RJ, et al. B-cell depletion with rituximab in relapsing-remitting multiple sclerosis. New Eng J Med. 2008; 358(7): 676-88.
- Dehghan L, Faraji F, Dalvand H, Shamsoddini A, Hadian-Rasanani MR, Aajami Z, et al. Occupational performance of individuals with Multiple Sclerosis based on disability level in Iran. Iran J Neurol. 2019; 18(1): 1-6.
- Farrokhi M, Moeini P, Fazilati M, Nazem H, Faraji S, Saadatpour Z, et al. Polymorphisms in CD14 gene may modify soluble CD14 levels and represent risk factors for multiple sclerosis. immunol investig. 2016; 12(2): 1-8.
- Milo R, Kahana E. Multiple sclerosis: geoepidemiology, genetics and the enviro-nment. Autoimmunity Rev. 2010; 9(5): 387-94.
- Gourraud PA, Harbo HF, Hauser SL, Baranzini SE. The genetics of multiple sclerosis: an up to date review. Immunol Rev. 2012; 248(1): 87-103.
- Waschbisch A, Atiya M, Linker RA, Potapov S, Schwab S, Derfuss T. Glatiramer acetate treatment normalizes deregulated microRNA expression in relapsing remitting multiple sclerosis. PloS One 2011; 6(9): 24-60.
- Nateghi B, Behshood P, Fathullahzadeh S, Mardanshah O. Circulating miR-95 is a potential biomarker of chronic lymphocytic leukemia. Res Mol Med. 2018; 26(6): 1-8.
- Namazi F, Hadi N, Moghimi M, Eshaghiyan A, Nateghi B. Down-regulation of miR-193b-3p and miR-376a-3p in chronic lymphocytic leukemia. Res Mol Med. 2019; 19(3): 45-53.
- Nateghi B, Shams E, Behshood P, Fathullahzadeh S, Salehi M. Expression profiles of miR-93 and miR-330 in iranian patients with chronic lymphocytic leukemia. Int J Med Lab. 2019; 6(2): 100-106.
- Vistbakka J, Elovaara I, Lehtimäki T, Hagman S. Circulating microRNAs as biomarkers in progressive multiple sclerosis. Multiple Sclerosis J. 2017; 23(3): 403-12.
- Freiesleben S, Hecker M, Zettl UK, Fuellen G, Taher L. Analysis of microRNA and gene expression profiles in multiple sclerosis: integrating interaction data to uncover regulatory mechanisms. Scientific Rep. 2016; 3(6): 34-51.
- Dweep H, Gretz N, Sticht C. miRWalk database for miRNA-target interactions. RNA Map. 2014; 23(1): 289-305.
- McDonald WI, Compston A, Edan G, Goodkin D, Hartung HP, Lublin FD, et al. Recommended diagnostic criteria for multiple sclerosis: guidelines from the International Panel on the diagnosis of multiple sclerosis. Annals of Neurology. Official J Am Neurol Associ Child Neurol Society 2001; 50(1): 121-27.
- Livak KJ, Schmittgen TD. Analysis of relative gene expression data using real-time quantitative PCR and the 2−ΔΔCT method. methods 2001; 25(4): 402-8.
- Hauser SL, Oksenberg JR, Baranzini SE. Multiple sclerosis. Rosenberg's Mol Genet Basis Neurologic Psychiatr Dis. 2015: 6(1): 1001-1014.
- Keller A, Leidinger P, Lange J, Borries A, Schroers H, Scheffler M, et al. Multiple sclerosis: microRNA expression profiles accurately differentiate patients with relapsing-remitting disease from healthy controls. PloS One 2009; 4(10): 40-74.
- Guerau-de-Arellano M, Alder H, Ozer HG, Lovett-Racke A, Racke MK. miRNA profiling for biomarker discovery in multiple sclerosis: from microarray to deep sequencing. J neuroimmunol. 2012; 248(2): 32-9.
- Lucherini OM, Obici L, Ferracin M, Fulci V, McDermott MF, Merlini G, et al. First report of circulating microRNAs in tumour necrosis factor receptor-associated periodic syndrome (TRAPS). PloS One 2013; 8(9): 34-43.
- Melkamu T, Zhang X, Tan J, Zeng Y, Kassie F. Alteration of microRNA expression in vinyl carbamate-induced mouse lung tumors and modulation by the chemopreventive agent indole-3-carbinol. Carcinogenesis 2009; 31(2): 252-58.
- Wang Q, Wang Y, Minto AW, Wang J, Shi Q, Li X, et al. MicroRNA-377 is up-regulated and can lead to increased fibronectin production in diabetic nephropathy. FASEB J. 2008; 22(12): 26-35.
- Ma X, Zhou J, Zhong Y, Jiang L, Mu P, Li Y, et al. Expression, regulation and function of microRNAs in multiple sclerosis. Int J Med Sci. 2014; 11(8): 810.
- Wu T, Chen G. miRNAs participate in MS pathological processes and its therapeutic response. Mediators Inflamm. 2016; 20(16): 19-25.
- Shen N, Liang D, Tang Y, De Vries N, Tak PP. MicroRNAs-novel regulators of systemic lupus erythematosus pathogenesis. Nat Reviews Rheumatol. 2012; 8(12): 70-81.










































 , Faezeh Namazi
, Faezeh Namazi 

 , Fatemeh Ketabchi
, Fatemeh Ketabchi 

 , Farinaz Khosravian
, Farinaz Khosravian 

 , Parisa Ravaghi
, Parisa Ravaghi 
 , Mansoor Salehi *
, Mansoor Salehi *