Sat, Feb 7, 2026
[Archive]
Volume 7, Issue 3 (August 2020)
IJML 2020, 7(3): 224-230 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Mazhab-Jafari K, Rouhandeh R, Bahrami R, Shahrivar F. Mass Investigation on Intestinal Parasite Infection in Masjed Soleyman, Iran, 2010-2017: A Large Population Survey. IJML 2020; 7 (3) :224-230
URL: http://ijml.ssu.ac.ir/article-1-337-en.html
URL: http://ijml.ssu.ac.ir/article-1-337-en.html
Department of Laboratory Sciences, Abadan Faculty of Medical Sciences, Abadan, Iran
Keywords: Intestinal Diseases, Parasitic Infections, Giardia lamblia, Hymenolepis nana, Epidemiology
Full-Text [PDF 260 kb]
(972 Downloads)
| Abstract (HTML) (1900 Views)
Introduction
References
Full-Text: (921 Views)
Introduction
Intestinal parasitic infections are one of the main sources of the infectious diseases that were reported in many different parts of the world, especially in tropical and subtropical areas. According to the World Health Organization (WHO), about 3.5 billion people in the world are affected by intestinal parasitic infections, and 450 million people have developed clinical symptoms. [1]. These infections could be transmitted to the human body in different ways and lead to various diseases to humans. Polluted water, contact with soil, food, and hygiene non-compliance are considered as pathways for transmission of infectious parasites to humans [2, 3]. The high prevalence of intestinal parasites in individuals, especially in children, depends on many factors, particularly personal and public hygiene [4]. These infections disrupt the absorption of food and other substances that are needed for the body. The intestinal parasite harms the body in different ways such as mechanical damage, toxic secretion, hematophagous, various lesions such as tissue damage through feeding and reproduction activities, anemia, loss of growth and weight, reduced individual activity, mental and psychological impairment, and many other symptoms. These problems depend on the immunologic, physiological, host, and socio-demographic factors. Intestinal parasite infections generally have a prolonged period, and in the absence of complete diagnosis and treatment, the patients become asymptomatic carriers of the parasite, start to spread the pathogens in the community, and endangering the public health [5, 6]. Since there are many documents on soil, food, and water contamination in many parts of Iran, people are at high risk of being contaminated with pathogenic parasites [7-13]. The fact that the spread and development of diseases’ benchmark could be unique in each region, the parasitic infections would be different in Iran by considering different ecological, social, economic, and cultural variety [14-20].
This cross-sectional and retrospective study investigated the frequency of intestinal parasites in Masjed Soleyman, Iran.
Materials and Methods
This study is a retrospective cross-sectional study. Data were collected from patients referring to the three medical centers in Masjed Soleyman, Iran, from 2010 to 2017. The city of Masjed Soleyman is located in the southwest of Iran and northeast of Khuzestan Province among the Zagros Mountains. It is hot and dry, with a population of 113,000 people, according to the latest census [21]. Part of the population of the city are nomads who migrate to this area during the cold season.
In these medical centers, the stool samples were collected, and each patient’s data were documented. The samples were examined by parasitology conventional methods such as microscopy observation for detecting blood, mucus, worms and protozoan parasites using Lugol’s iodine solution or physiological saline. Also, in some cases, additional testing by the formaldehyde-ether sedimentation and modified acid-fast staining techniques have been applied if it is required. The data registered in laboratory records include the patient’s name, gender, date, and parasitology test results. Patient’s records were collected and classified with respecting ethical principles and without mentioning their names.
Statistical analysis
The collected data were analyzed with SPSS version 16 [22] by descriptive statistics methods such as absolute frequency and relative frequency percent. Also, the analytical statistics methods, such as Chi-square, were applied. The significance level of the test was 0.05. The research project has been approved by the code “94st-0024” and with the ethics code of IR.ABADANUMS.REC.1394.42 at the Abadan Faculty of Medical Sciences, Abadan, Iran.
Results
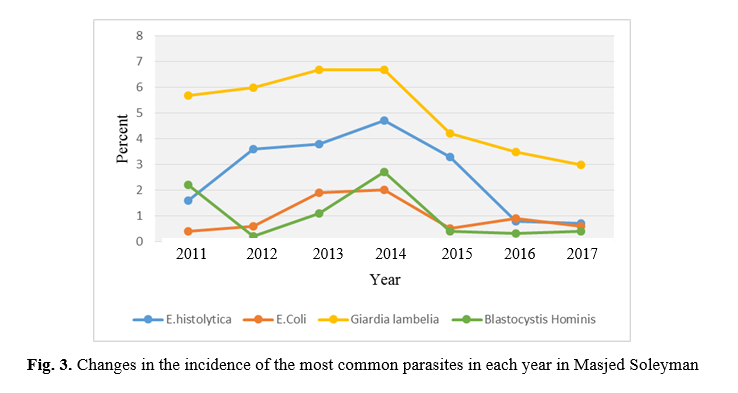
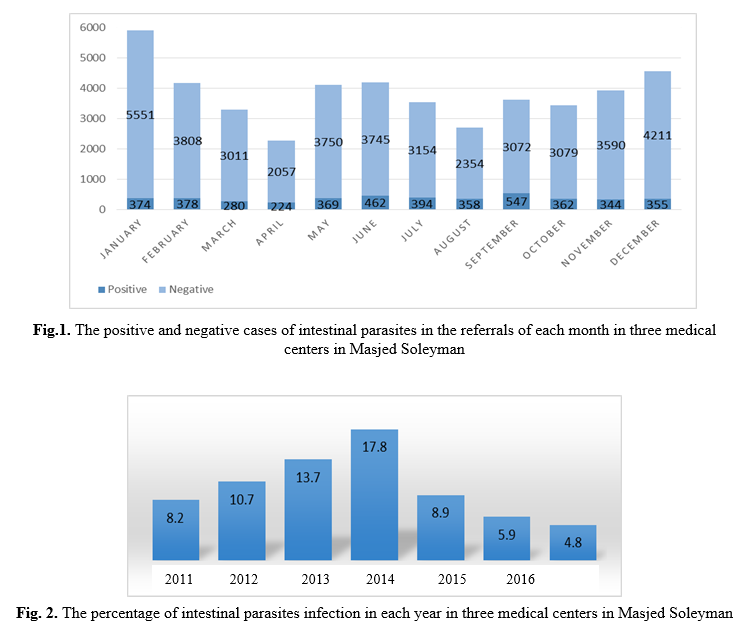
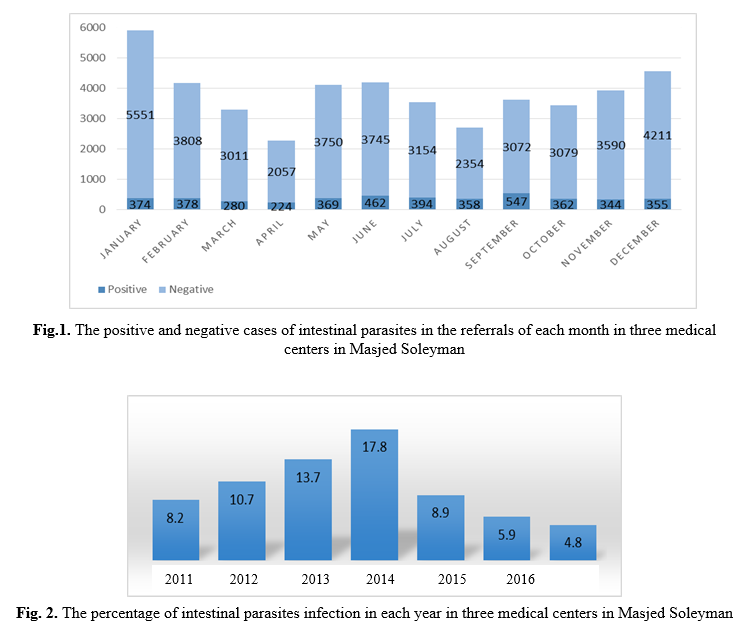
In the three medical centers, the stool test was done by the direct method using Lugol’s iodine solution or physiological saline. From 2010 to 2017, the data were collected from 45,829 registered individuals. Survey data showed that 30,050 people were male (65.6%), and 15,779 were female (34.4%). The surveys indicate that 4,447 people (9.7%) were infected with intestinal parasites. The analysis revealed that there is a significant relationship between the rate of infection with intestinal parasites and the sex of individuals (p<0.001). Table 1 shows the infection rate for each parasite by gender. The relationship between infection and seasons is significant, as well (p<0.001). Table 2 illustrates the number and percentage of positive intestinal parasites in each season. The results of intestinal parasites in the referals of each month are presented in Fig. 1. The percentage of intestinal parasites infection were 4.8 in 2017 and 17.8 in 2014 (Fig. 2). Incidence of each most common parasites in each year is shown in Fig. 3.
This cross-sectional and retrospective study investigated the frequency of intestinal parasites in Masjed Soleyman, Iran.
Materials and Methods
This study is a retrospective cross-sectional study. Data were collected from patients referring to the three medical centers in Masjed Soleyman, Iran, from 2010 to 2017. The city of Masjed Soleyman is located in the southwest of Iran and northeast of Khuzestan Province among the Zagros Mountains. It is hot and dry, with a population of 113,000 people, according to the latest census [21]. Part of the population of the city are nomads who migrate to this area during the cold season.
In these medical centers, the stool samples were collected, and each patient’s data were documented. The samples were examined by parasitology conventional methods such as microscopy observation for detecting blood, mucus, worms and protozoan parasites using Lugol’s iodine solution or physiological saline. Also, in some cases, additional testing by the formaldehyde-ether sedimentation and modified acid-fast staining techniques have been applied if it is required. The data registered in laboratory records include the patient’s name, gender, date, and parasitology test results. Patient’s records were collected and classified with respecting ethical principles and without mentioning their names.
Statistical analysis
The collected data were analyzed with SPSS version 16 [22] by descriptive statistics methods such as absolute frequency and relative frequency percent. Also, the analytical statistics methods, such as Chi-square, were applied. The significance level of the test was 0.05. The research project has been approved by the code “94st-0024” and with the ethics code of IR.ABADANUMS.REC.1394.42 at the Abadan Faculty of Medical Sciences, Abadan, Iran.
Results
In the three medical centers, the stool test was done by the direct method using Lugol’s iodine solution or physiological saline. From 2010 to 2017, the data were collected from 45,829 registered individuals. Survey data showed that 30,050 people were male (65.6%), and 15,779 were female (34.4%). The surveys indicate that 4,447 people (9.7%) were infected with intestinal parasites. The analysis revealed that there is a significant relationship between the rate of infection with intestinal parasites and the sex of individuals (p<0.001). Table 1 shows the infection rate for each parasite by gender. The relationship between infection and seasons is significant, as well (p<0.001). Table 2 illustrates the number and percentage of positive intestinal parasites in each season. The results of intestinal parasites in the referals of each month are presented in Fig. 1. The percentage of intestinal parasites infection were 4.8 in 2017 and 17.8 in 2014 (Fig. 2). Incidence of each most common parasites in each year is shown in Fig. 3.
Table 1. Infection rate for each parasite by gender in three medical centers in Masjed Soleyman
| Parasites | Gender | Total | Positive cases (%) | Whole tested patients (%) | |
| Male | Female | ||||
| Giardia lamblia | 1593 | 1010 | 2603 | 58.5 | 5.7 |
| Entamoebahistolytica/ dispar | 589 | 561 | 1150 | 25.9 | 2.5 |
| Entamoeba coli | 176 | 144 | 320 | 7.2 | 0.7 |
| Blastocystishominis | 97 | 71 | 168 | 3.8 | 0.4 |
| Chilomastixmesnili | 60 | 17 | 77 | 1.73 | 0.17 |
| Hymonlepsis Nana | 48 | 20 | 68 | 1.53 | 0.15 |
| Endolimax Nana | 18 | 24 | 42 | 0.94 | 0.09 |
| Iodamoeba Butschlii | 0 | 8 | 8 | 0.18 | 0.02 |
| Enrerobius Vermicnlaris | 3 | 4 | 7 | 0.14 | 0.01 |
| Trichomonas Hominis | 1 | 1 | 2 | 0.04 | 0.004 |
| Strongyloides Stercoralis | 1 | 1 | 2 | 0.04 | 0.004 |
| Total | 2586 | 1861 | 4447 | 100 | 9.7 |
Table 2. The number and percentage of the tested samples positive intestinal parasites observed in each season in Masjed Soleyman
| Season | Tested samples (%) | Positive samples (%) |
| Spring | 10607 (23.1) | 1055 (23.7) |
| Summer | 9879 (21.6) | 1299 (29.2) |
| Autumn | 11941 (26.1) | 1061 (23.9) |
| Winter | 13402 (29.2) | 1032 (23.2) |
| Total | 45829 (100) | 4447 (100) |
Discussion
The parasites are transmitted to humans in various ways, including polluted water, food, soil, and dust, which are contacted with infected patients, and could cause human infection. The prevalence of parasitic infections is related to factors such as the geographical situation, the lifestyle, the economic and health situation of people, and any of these factors could fluctuate the prevalence rate [23, 24].
In the present study, the prevalence of intestinal parasite is 9.7%, which is 5.6% for males and 4.1% for females. In other words, 58.2% of people infected with parasites were male, and 41.8% were female. It is found in this study that the rate of parasitic infection in men is higher than women. The statistical analysis of this issue has revealed that the difference between males and females is significant in the aspect of intestinal parasites infection.
The results of this study are demonstrated in Table 2 shows that most of the parasitic infections happened in summer, which are 1,299 (29.2%) cases, and the lowest rate occurred in winter, which is 1,032 (23.2%) cases. The statistical analysis, which is done by the Chi-square test indicated that there is a significant relationship between the incidence of parasitic infections and season. According to table 2, most cases referring to Masjed Soleyman medical centers happened in the autumn and winter. This increase is related to referrals to medical centers, where the increase in the population is due to the migration of nomads in cold seasons. However, the incidence of parasitic infections in winter is less than the warm seasons.
The intestinal parasites infection is 4.7% in Karaj, 6.2% in Dezful, 10.42% in Isfahan, 10.6% in Tehran, 12% in Ahvaz, 14.1% in Ilam, 32.7% in Roudehen and 37.5% in rural areas of Boyer-Ahmad [14-16, 18, 19, 25, 26]. Furthermore, in the similar studies, the intestinal parasite’s infection is 3.7% in Turkey, 5.93% in Qatar, 8.9% in India, 14.71% in Italy, 17.5% in Brazil, 24.6% in Malaysia and 44% in Jordan [27-33].
The most common observed parasite in this study was Giardia lamblia (58.5% of positive cases). The transmission of this parasite is direct and with no need for any intermediate host. In other studies, the most reported parasites were protozoan parasites [14-19, 25-33].
Infection with intestinal parasites has declined in this region since the year 2014. According to the results of Figs. 2 and 3, all parasitic infections have been reduced. As can be seen, the parasitic infections had declined from 17.8% in 2014 to 4.8% in 2017.
The most crucial protozoan parasites observed in this study are Giardia lamblia, Entamoeba histolytica/dispar, Entamoeba coli, and Blastocystis hominis. Fig. 3 shows changes in the incidence of these parasites during the study period. It reveals that the number of infections of these parasites has been significantly reduced since the year 2014.
In the current study, it was found that 98.3% of infected people have protozoan parasites, and 1.7% are infected with worm parasites. According to the actions done to improve the quality of public health in Iran, it seems that actions cause a decrease in worm parasite infections. This decrease has happened in Hymenolepis nana. The status of infection was decreasing for seven years. The rate of infection of Hymenolepis nana was decreased from 0.5% in 2010 to 0.04% in 2017.
Conclusion
According to the information obtained in this study, it was determined that the protozoan parasite infections happen more than worm infections. The most common parasites observed in this study are Giardia lamblia and Amoebas. It should be noted that these infections spread directly in the community without the need for any intermediate host. Polluted water and food could infect people with intestinal parasite infections. Patients’ gender and seasons are effective factors in the prevalence of intestinal parasitic infections in this area. Due to the presence of nomads in Masjed Soleyman in the cold seasons of the year, the risk of parasite transmission is higher. Considering the unique conditions in this area, special measures should be taken to control the diseases.
Conflict of Interest
The authors declare that they have no competing interests.
Acknowledgments
The authors would like to express their gratitude to all colleagues in the medical centers of Masjed Soleyman for their collaboration in performing the tests and providing all the data.
In the present study, the prevalence of intestinal parasite is 9.7%, which is 5.6% for males and 4.1% for females. In other words, 58.2% of people infected with parasites were male, and 41.8% were female. It is found in this study that the rate of parasitic infection in men is higher than women. The statistical analysis of this issue has revealed that the difference between males and females is significant in the aspect of intestinal parasites infection.
The results of this study are demonstrated in Table 2 shows that most of the parasitic infections happened in summer, which are 1,299 (29.2%) cases, and the lowest rate occurred in winter, which is 1,032 (23.2%) cases. The statistical analysis, which is done by the Chi-square test indicated that there is a significant relationship between the incidence of parasitic infections and season. According to table 2, most cases referring to Masjed Soleyman medical centers happened in the autumn and winter. This increase is related to referrals to medical centers, where the increase in the population is due to the migration of nomads in cold seasons. However, the incidence of parasitic infections in winter is less than the warm seasons.
The intestinal parasites infection is 4.7% in Karaj, 6.2% in Dezful, 10.42% in Isfahan, 10.6% in Tehran, 12% in Ahvaz, 14.1% in Ilam, 32.7% in Roudehen and 37.5% in rural areas of Boyer-Ahmad [14-16, 18, 19, 25, 26]. Furthermore, in the similar studies, the intestinal parasite’s infection is 3.7% in Turkey, 5.93% in Qatar, 8.9% in India, 14.71% in Italy, 17.5% in Brazil, 24.6% in Malaysia and 44% in Jordan [27-33].
The most common observed parasite in this study was Giardia lamblia (58.5% of positive cases). The transmission of this parasite is direct and with no need for any intermediate host. In other studies, the most reported parasites were protozoan parasites [14-19, 25-33].
Infection with intestinal parasites has declined in this region since the year 2014. According to the results of Figs. 2 and 3, all parasitic infections have been reduced. As can be seen, the parasitic infections had declined from 17.8% in 2014 to 4.8% in 2017.
The most crucial protozoan parasites observed in this study are Giardia lamblia, Entamoeba histolytica/dispar, Entamoeba coli, and Blastocystis hominis. Fig. 3 shows changes in the incidence of these parasites during the study period. It reveals that the number of infections of these parasites has been significantly reduced since the year 2014.
In the current study, it was found that 98.3% of infected people have protozoan parasites, and 1.7% are infected with worm parasites. According to the actions done to improve the quality of public health in Iran, it seems that actions cause a decrease in worm parasite infections. This decrease has happened in Hymenolepis nana. The status of infection was decreasing for seven years. The rate of infection of Hymenolepis nana was decreased from 0.5% in 2010 to 0.04% in 2017.
Conclusion
According to the information obtained in this study, it was determined that the protozoan parasite infections happen more than worm infections. The most common parasites observed in this study are Giardia lamblia and Amoebas. It should be noted that these infections spread directly in the community without the need for any intermediate host. Polluted water and food could infect people with intestinal parasite infections. Patients’ gender and seasons are effective factors in the prevalence of intestinal parasitic infections in this area. Due to the presence of nomads in Masjed Soleyman in the cold seasons of the year, the risk of parasite transmission is higher. Considering the unique conditions in this area, special measures should be taken to control the diseases.
Conflict of Interest
The authors declare that they have no competing interests.
Acknowledgments
The authors would like to express their gratitude to all colleagues in the medical centers of Masjed Soleyman for their collaboration in performing the tests and providing all the data.
References
[1]. World Health Organization. Control of Tropical Diseases. Switzerland: Geneva, WHO; 1998.
[2]. Daryani A, Sharif M, Nasrolahei M, Khalilian A, Mohammadi A, Barzegar G. Epidemiological survey of the prevalence of intestinal parasites among schoolchildren in Sari, northern Iran. Trans R Soc Trop Med Hyg. 2012; 106(8): 455-59.
[3]. Turki H, Hamedi Y, Heidari-Hengami M, Najafi-Asl M, Rafati S, Sharifi-Sarasiabi K. Prevalence of intestinal parasitic infection among primary school children in southern Iran. J Parasit Dis. 2016; 5(1): 17-22.
[4]. Taheri F, Namakin K, Zarban A, Sharifzadeh G. Intestinal parasitic infection among school children in South Khorasan Province, Iran. J Res Health Sci. 2011; 11(1): 45-50.
[5]. Saebi E. Textbook of Clinical Parasitology. 2th ed. Tehran: Aeig; 2009.
[6]. Mahmud MA, Spigt M, Bezabih AM, Pavon IL, Dinant GJ, Velasco RB. Efficacy of handwashing with soap and nail clipping on intestinal parasitic infections in school-aged children: a factorial cluster randomized controlled trial. PLoS Med. 2015; 12(6): 1001837.
[7]. Shahnazi M, Jafari-Sabet M. Prevalence of parasitic contamination of raw vegetables in villages of Qazvin Province, Iran. Foodborne Pathogens and Disease 2010; 7(9): 1025-30.
[8]. Fallah AA, Pirali-Kheirabadi K, Shirvani F, Saei-Dehkordi SS. Prevalence of parasitic contamination in vegetables used for raw consumption in Shahrekord, Iran: influence of season and washing procedure. Food Control. 2012; 25(2): 617-20.
[9]. Mohaghegh MA, Jafari R, Ghomashlooyan M, Mirzaei F, Azami M, Falahati M, et al. Soil Contamination With Oocysts of Crypto-sporidium spp. in Isfahan, Central Iran. Int J Enteric Pathog. 2015; 3(3): 1-5.
[10]. Maraghi S, Mazhab Jafari K, Sadjjadi SM, Latifi SM, Zibaei M. Study on the contamination of Abadan public parks soil with Toxocara spp. eggs. J Environ Health Sci Eng. 2014; 12(1): 86.
[11]. Mazhab-Jafari K, Zibaei M, Maraghi S, Rouhandeh R, Helichi M, Ghafeli-Nejad M, et al. Prevalence of Toxocara eggs in the soil of public parks of Khorramshahr city, southwest Iran. Ann Parasitol. 2019; 65(4): 351-56.
[12]. Rafiei A, Rahdar M, Valipour Nourozi R. Isolation and identification of parasitic protozoa in sampled water from the southwest of Iran. Jundishapur J Health Sci. 2014; 6(4): 23462.
[13]. Mahmoudi M, Ashrafi K, Abedinzadeh H, Tahvildar-Bideruni F, Haghighi A, Bandehpour M, et al. Development of sensitive detection of cryptosporidium and Giardia from surface water in iran. Iran J Parasitol. 2011; 6(3): 43-51.
[14]. Fasihi-Karami M, Mazhab-Jafari K, Rouhandeh R, Shahrivar F, Karbalaei R, Beigzadeh E, et al. Epidemiologic study of intestinal parasitic infections in Ahvaz, southwest Iran in 2010-2015. Arvand J Health Med Sci. 2017; 2(1): 15-21.
[15]. Maniey M, Maraghi S, Mazhabjafari K. Study the frequency of intestinal parasitic infection in patients referred to central laboratory of Great Dezful hospital in 2010 and 2011. Jundishapur J Health Sci. 2012; 4(2): 31-8.
[16]. Nasiri V, Esmailnia K, Karim G, Nasir M, Akhavan O. Intestinal parasitic infections among inhabitants of Karaj City, Tehran province, Iran in 2006-2008. Korean J Parasitol. 2009; 47(3): 265-8.
[17]. Arani AS, Alaghehbandan R, Akhlaghi L, Shahi M, Lari AR. Prevalence of intestinal parasites in a population in south of Tehran, Iran. Rev Inst Med Trop Sao Paulo. 2008; 50(3): 145-49.
[18]. Hemmati N, Razmjou E, Hashemi-Hafshejani S, Motevalian A, Akhlaghi L, Meamar AR. Prevalence and risk factors of human intestinal parasites in roudehen, Tehran Province, Iran. Iran J Parasitol. 2017; 12(3): 364-73.
[19]. Sarkari B, Hosseini G, Motazedian MH, Fararouei M, Moshfe A. Prevalence and risk factors of intestinal protozoan infections: a population-based study in rural areas of Boyer-Ahmad district, Southwestern Iran. BMC Infect Dis. 2016; 16(1): 703.
[20]. Tork M, Sharif M, Yazdani Charati J, Nazar I, Hosseini SA. Prevalence of intestinal parasitic infections and associated risk factors in west of mazandaran province, Iran. J Mazandaran Univ Med Sci. 2016; 25(134): 81-8.
[21]. Statistical Centre of Iran [cited 2017]. Available from: http://www.amar.org.ir.
[22].SpssInc. IBM SPSS Statistics for Windows. 16 ed. Chicago: SPSS Inc; 2007.
[23]. Mahmoud A, Mandell J, Bennett J, Dolin R. Introduction to helminth infection in: Principles and practice of infection diseases. 5th ed. New York: Churchill livingstone; 2000.
[24]. Harrisons. Principles of internal medicine, Protozoa and helminthic infections. New York: MC Grow-Hill; 2001. p. 1185-236
[25]. Jafari R, Sharifi F, Bagherpour B, Safari M. Prevalence of intestinal parasites in Isfahan city, central Iran, 2014. J Parasit Dis. 2016; 40(3): 679-82.
[26]. Viesy S, Abdi J, Rezaei Z. What are hidden facts behind intestinal parasitic infections in ilam city? Infect Disord Drug Targets 2019; 19(3): 284-87.
[27]. Selek MB, Bektore B, Karagoz E, Baylan O, Ozyurt M. Distribution of parasites detected in stool samples of patients admitted to our parasitology laboratory during a three-year period between 2012 and 2014. Turkiye Parazitol Derg 2016; 40(3): 137-40.
[28]. Abu-Madi MA, Behnke JM, Boughattas S, Al-Thani A, Doiphode SH. A decade of intestinal protozoan epidemiology among settled immigrants in Qatar. BMC Infect Dis. 2016; 16: 370.
[29]. Praharaj I, Sarkar R, Rao Ajjampur SS, Roy S, Kang G. Temporal trends of intestinal parasites in patients attending a tertiary care hospital in south India: A seven-year retrospective analysis. Indian J Med Res. 2017; 146(1): 111-20.
[30]. Bartolini A, Zorzi G, Besutti V. Prevalence of intestinal parasitoses detected in Padua teaching hospital, Italy, March 2011-February 2013. Infez Med. 2017; 25(2): 133-41.
[31]. Faria CP, Zanini GM, Dias GS, da Silva S, de Freitas MB, Almendra R, et al. Geospatial distribution of intestinal parasitic infections in Rio de Janeiro (Brazil) and its association with social determinants. PLoS Negl Trop Dis. 2017; 11(3): 5445.
[32]. Sinniah B, Hassan AK, Sabaridah I, Soe MM, Ibrahim Z, Ali O. Prevalence of intestinal parasitic infections among communities living in different habitats and its comparison with one hundred and one studies conducted over the past 42 years (1970 to 2013) in Malaysia. Trop Biomed. 2014; 31(2): 190-206.
[33]. Jaran AS. Prevalence and seasonal variation of human intestinal parasites in patients attending hospital with abdominal symptoms in northern Jordan. East Mediterr Health J. 2017; 22(10): 756-60.
[2]. Daryani A, Sharif M, Nasrolahei M, Khalilian A, Mohammadi A, Barzegar G. Epidemiological survey of the prevalence of intestinal parasites among schoolchildren in Sari, northern Iran. Trans R Soc Trop Med Hyg. 2012; 106(8): 455-59.
[3]. Turki H, Hamedi Y, Heidari-Hengami M, Najafi-Asl M, Rafati S, Sharifi-Sarasiabi K. Prevalence of intestinal parasitic infection among primary school children in southern Iran. J Parasit Dis. 2016; 5(1): 17-22.
[4]. Taheri F, Namakin K, Zarban A, Sharifzadeh G. Intestinal parasitic infection among school children in South Khorasan Province, Iran. J Res Health Sci. 2011; 11(1): 45-50.
[5]. Saebi E. Textbook of Clinical Parasitology. 2th ed. Tehran: Aeig; 2009.
[6]. Mahmud MA, Spigt M, Bezabih AM, Pavon IL, Dinant GJ, Velasco RB. Efficacy of handwashing with soap and nail clipping on intestinal parasitic infections in school-aged children: a factorial cluster randomized controlled trial. PLoS Med. 2015; 12(6): 1001837.
[7]. Shahnazi M, Jafari-Sabet M. Prevalence of parasitic contamination of raw vegetables in villages of Qazvin Province, Iran. Foodborne Pathogens and Disease 2010; 7(9): 1025-30.
[8]. Fallah AA, Pirali-Kheirabadi K, Shirvani F, Saei-Dehkordi SS. Prevalence of parasitic contamination in vegetables used for raw consumption in Shahrekord, Iran: influence of season and washing procedure. Food Control. 2012; 25(2): 617-20.
[9]. Mohaghegh MA, Jafari R, Ghomashlooyan M, Mirzaei F, Azami M, Falahati M, et al. Soil Contamination With Oocysts of Crypto-sporidium spp. in Isfahan, Central Iran. Int J Enteric Pathog. 2015; 3(3): 1-5.
[10]. Maraghi S, Mazhab Jafari K, Sadjjadi SM, Latifi SM, Zibaei M. Study on the contamination of Abadan public parks soil with Toxocara spp. eggs. J Environ Health Sci Eng. 2014; 12(1): 86.
[11]. Mazhab-Jafari K, Zibaei M, Maraghi S, Rouhandeh R, Helichi M, Ghafeli-Nejad M, et al. Prevalence of Toxocara eggs in the soil of public parks of Khorramshahr city, southwest Iran. Ann Parasitol. 2019; 65(4): 351-56.
[12]. Rafiei A, Rahdar M, Valipour Nourozi R. Isolation and identification of parasitic protozoa in sampled water from the southwest of Iran. Jundishapur J Health Sci. 2014; 6(4): 23462.
[13]. Mahmoudi M, Ashrafi K, Abedinzadeh H, Tahvildar-Bideruni F, Haghighi A, Bandehpour M, et al. Development of sensitive detection of cryptosporidium and Giardia from surface water in iran. Iran J Parasitol. 2011; 6(3): 43-51.
[14]. Fasihi-Karami M, Mazhab-Jafari K, Rouhandeh R, Shahrivar F, Karbalaei R, Beigzadeh E, et al. Epidemiologic study of intestinal parasitic infections in Ahvaz, southwest Iran in 2010-2015. Arvand J Health Med Sci. 2017; 2(1): 15-21.
[15]. Maniey M, Maraghi S, Mazhabjafari K. Study the frequency of intestinal parasitic infection in patients referred to central laboratory of Great Dezful hospital in 2010 and 2011. Jundishapur J Health Sci. 2012; 4(2): 31-8.
[16]. Nasiri V, Esmailnia K, Karim G, Nasir M, Akhavan O. Intestinal parasitic infections among inhabitants of Karaj City, Tehran province, Iran in 2006-2008. Korean J Parasitol. 2009; 47(3): 265-8.
[17]. Arani AS, Alaghehbandan R, Akhlaghi L, Shahi M, Lari AR. Prevalence of intestinal parasites in a population in south of Tehran, Iran. Rev Inst Med Trop Sao Paulo. 2008; 50(3): 145-49.
[18]. Hemmati N, Razmjou E, Hashemi-Hafshejani S, Motevalian A, Akhlaghi L, Meamar AR. Prevalence and risk factors of human intestinal parasites in roudehen, Tehran Province, Iran. Iran J Parasitol. 2017; 12(3): 364-73.
[19]. Sarkari B, Hosseini G, Motazedian MH, Fararouei M, Moshfe A. Prevalence and risk factors of intestinal protozoan infections: a population-based study in rural areas of Boyer-Ahmad district, Southwestern Iran. BMC Infect Dis. 2016; 16(1): 703.
[20]. Tork M, Sharif M, Yazdani Charati J, Nazar I, Hosseini SA. Prevalence of intestinal parasitic infections and associated risk factors in west of mazandaran province, Iran. J Mazandaran Univ Med Sci. 2016; 25(134): 81-8.
[21]. Statistical Centre of Iran [cited 2017]. Available from: http://www.amar.org.ir.
[22].SpssInc. IBM SPSS Statistics for Windows. 16 ed. Chicago: SPSS Inc; 2007.
[23]. Mahmoud A, Mandell J, Bennett J, Dolin R. Introduction to helminth infection in: Principles and practice of infection diseases. 5th ed. New York: Churchill livingstone; 2000.
[24]. Harrisons. Principles of internal medicine, Protozoa and helminthic infections. New York: MC Grow-Hill; 2001. p. 1185-236
[25]. Jafari R, Sharifi F, Bagherpour B, Safari M. Prevalence of intestinal parasites in Isfahan city, central Iran, 2014. J Parasit Dis. 2016; 40(3): 679-82.
[26]. Viesy S, Abdi J, Rezaei Z. What are hidden facts behind intestinal parasitic infections in ilam city? Infect Disord Drug Targets 2019; 19(3): 284-87.
[27]. Selek MB, Bektore B, Karagoz E, Baylan O, Ozyurt M. Distribution of parasites detected in stool samples of patients admitted to our parasitology laboratory during a three-year period between 2012 and 2014. Turkiye Parazitol Derg 2016; 40(3): 137-40.
[28]. Abu-Madi MA, Behnke JM, Boughattas S, Al-Thani A, Doiphode SH. A decade of intestinal protozoan epidemiology among settled immigrants in Qatar. BMC Infect Dis. 2016; 16: 370.
[29]. Praharaj I, Sarkar R, Rao Ajjampur SS, Roy S, Kang G. Temporal trends of intestinal parasites in patients attending a tertiary care hospital in south India: A seven-year retrospective analysis. Indian J Med Res. 2017; 146(1): 111-20.
[30]. Bartolini A, Zorzi G, Besutti V. Prevalence of intestinal parasitoses detected in Padua teaching hospital, Italy, March 2011-February 2013. Infez Med. 2017; 25(2): 133-41.
[31]. Faria CP, Zanini GM, Dias GS, da Silva S, de Freitas MB, Almendra R, et al. Geospatial distribution of intestinal parasitic infections in Rio de Janeiro (Brazil) and its association with social determinants. PLoS Negl Trop Dis. 2017; 11(3): 5445.
[32]. Sinniah B, Hassan AK, Sabaridah I, Soe MM, Ibrahim Z, Ali O. Prevalence of intestinal parasitic infections among communities living in different habitats and its comparison with one hundred and one studies conducted over the past 42 years (1970 to 2013) in Malaysia. Trop Biomed. 2014; 31(2): 190-206.
[33]. Jaran AS. Prevalence and seasonal variation of human intestinal parasites in patients attending hospital with abdominal symptoms in northern Jordan. East Mediterr Health J. 2017; 22(10): 756-60.
Type of Study: Research |
Subject:
Parasitology
Received: 2019/11/11 | Accepted: 2020/08/31 | Published: 2020/08/27
Received: 2019/11/11 | Accepted: 2020/08/31 | Published: 2020/08/27
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |